Cushing Syndrome, a condition resulting from prolonged exposure to high levels of cortisol, dramatically impacts various body systems. This hormonal imbalance, stemming from either adrenal gland tumors or external corticosteroid use, manifests in a wide array of symptoms, ranging from weight gain and fatigue to skin changes and weakened bones. Understanding the underlying causes, diagnostic processes, and treatment options is crucial for effective management and improving patient outcomes.
This comprehensive guide explores the complexities of Cushing Syndrome, detailing its physiological mechanisms, diagnostic approaches, available treatments, and strategies for managing associated complications. We will delve into the impact on different body systems, discuss risk factors and prevention methods, and present case studies to illustrate the diverse presentations of this condition. The aim is to provide a clear and informative resource for both healthcare professionals and individuals affected by Cushing Syndrome.
Definition and Characteristics of Cushing Syndrome
Cushing syndrome is a hormonal disorder characterized by prolonged exposure to high levels of cortisol. This excess cortisol can stem from various causes, leading to a wide range of symptoms affecting multiple body systems. Understanding the underlying mechanisms and diverse presentations of this syndrome is crucial for accurate diagnosis and effective management.
Physiological Mechanisms Underlying Cushing Syndrome
Cushing syndrome arises from the disruption of the hypothalamic-pituitary-adrenal (HPA) axis, the complex system regulating cortisol production. Normally, the hypothalamus releases corticotropin-releasing hormone (CRH), which stimulates the pituitary gland to produce adrenocorticotropic hormone (ACTH). ACTH then triggers the adrenal glands to release cortisol. In Cushing syndrome, this delicate balance is upset, resulting in excessive cortisol production. This excess cortisol can lead to a cascade of effects throughout the body, impacting metabolism, immune function, and many other processes.
The specific mechanisms involved depend on the underlying cause of the syndrome.
Types of Cushing Syndrome and Their Causes
Cushing syndrome can be broadly categorized into two main types: ACTH-dependent and ACTH-independent. ACTH-dependent Cushing syndrome results from excessive ACTH stimulation of the adrenal glands. This can be caused by pituitary adenomas (benign tumors of the pituitary gland producing excess ACTH), ectopic ACTH production (ACTH secretion from tumors outside the pituitary gland, such as lung or pancreatic cancers), or other less common causes.
ACTH-independent Cushing syndrome, on the other hand, is due to adrenal adenoma or carcinoma (tumors of the adrenal gland), resulting in autonomous cortisol production independent of ACTH stimulation. Exogenous Cushing syndrome is a separate category caused by prolonged use of high-dose corticosteroids, such as prednisone, for conditions like asthma or autoimmune diseases.
Common Symptoms Associated with Cushing Syndrome
The symptoms of Cushing syndrome are diverse and often nonspecific, making diagnosis challenging. Common symptoms include weight gain, particularly in the face (moon face), abdomen, and upper back (buffalo hump), along with easy bruising and thin, fragile skin. Muscle weakness and wasting (muscle atrophy) are also frequent complaints. Other symptoms can include hypertension (high blood pressure), high blood sugar (hyperglycemia), and increased susceptibility to infections.
Women may experience menstrual irregularities, while men may experience decreased libido and erectile dysfunction. Facial hair growth (hirsutism) is common in women. These symptoms vary in severity and presentation among individuals.
Comparison of Cushing Syndrome Symptoms with Similar Conditions
| Symptom | Cushing Syndrome | Hypothyroidism | Obesity |
|---|---|---|---|
| Weight Gain | Significant, often central obesity | May occur, but often less pronounced | Significant, often generalized |
| Fatigue | Present | Prominent | Can be present |
| Muscle Weakness | Significant, proximal muscle weakness | Present, often with myalgias | May occur due to inactivity |
| Skin Changes | Thinning skin, easy bruising, striae | Dry, coarse skin | May have stretch marks |
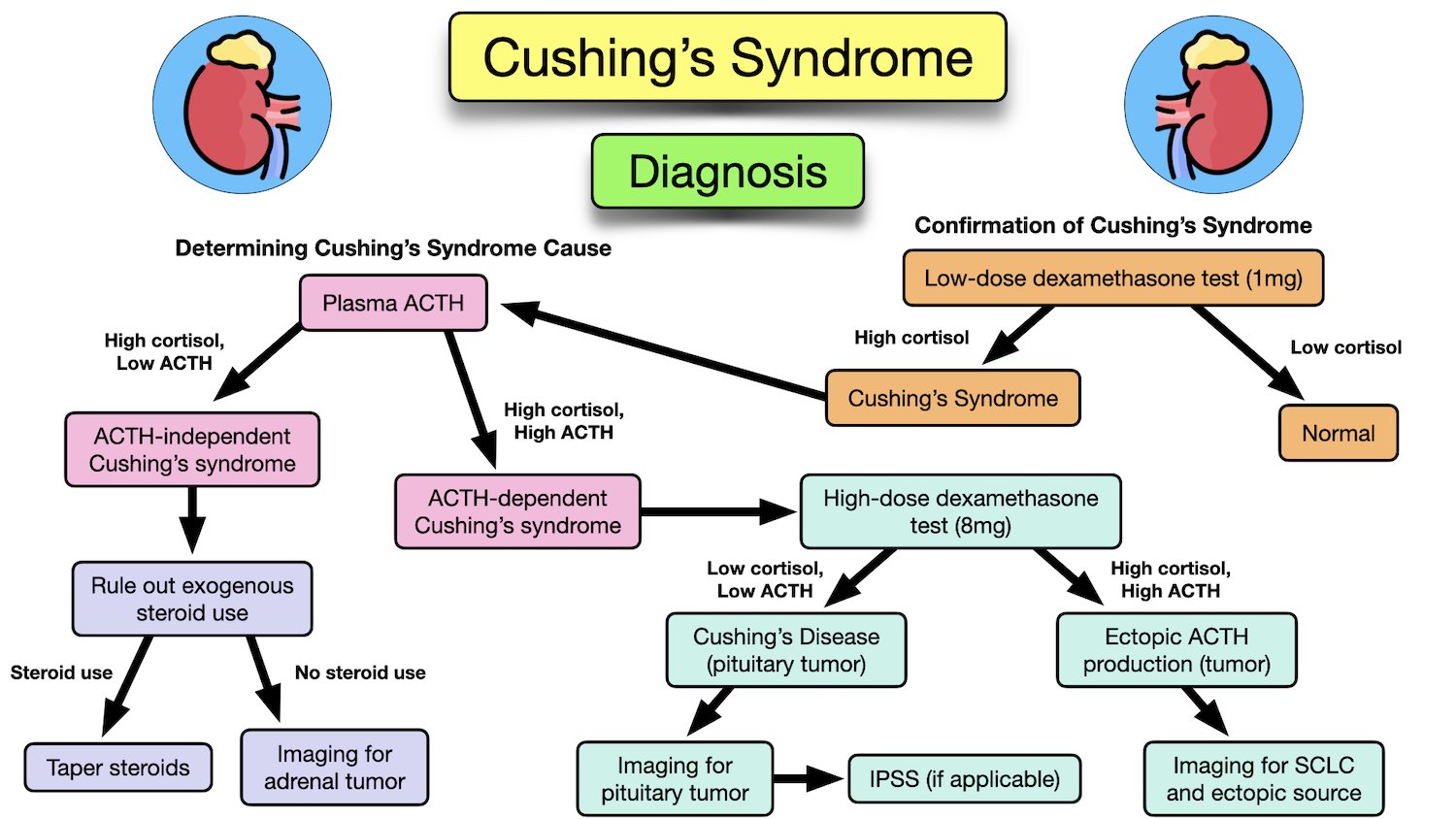
Diagnostic Procedures for Cushing Syndrome
Diagnosing Cushing syndrome requires a systematic approach involving several laboratory tests and imaging techniques to confirm the excess cortisol production and identify its cause. The diagnostic process can be complex due to the variability of symptoms and the potential for overlapping conditions. Accurate diagnosis is crucial for initiating appropriate treatment and improving patient outcomes.
Laboratory Tests for Cushing Syndrome
Several laboratory tests are used to assess cortisol levels and their regulation. These tests help determine if hypercortisolism is present and guide further investigations into the underlying cause. The initial screening often involves a 24-hour urine free cortisol test, which measures the total amount of cortisol excreted in the urine over a 24-hour period. Elevated levels suggest Cushing syndrome.
Further confirmation may involve a low-dose dexamethasone suppression test, which assesses the body’s ability to suppress cortisol production in response to dexamethasone, a synthetic glucocorticoid. Failure to suppress cortisol levels supports the diagnosis. Additional tests, such as the late-night salivary cortisol test, can provide further information about cortisol secretion patterns. Finally, measuring serum cortisol levels may also be used to provide a snapshot of cortisol levels at a particular point in time, although this alone is not sufficient for diagnosis.
Imaging Techniques in Cushing Syndrome Diagnosis
Imaging techniques play a crucial role in identifying the source of excess cortisol production. High-resolution computed tomography (CT) scans and magnetic resonance imaging (MRI) scans of the adrenal glands and pituitary gland are commonly used to visualize these organs and detect abnormalities such as adrenal adenomas or pituitary microadenomas. These imaging modalities provide detailed anatomical information, allowing for the precise localization of potential tumors or other lesions responsible for hypercortisolism.
In some cases, a positron emission tomography (PET) scan might be used to detect tumors with increased metabolic activity. The choice of imaging technique depends on the suspected location of the underlying cause and the availability of resources.
Interpreting Diagnostic Results and Challenges
Interpreting diagnostic results for Cushing syndrome can be challenging due to the complexity of the endocrine system and the potential for overlapping symptoms with other conditions. For instance, false-positive results can occur in conditions such as obesity, depression, and certain medications. Conversely, false-negative results can arise if the testing is not performed correctly or if the excess cortisol production is intermittent.
The diagnosis often requires a combination of laboratory tests and imaging studies, along with a thorough clinical evaluation to integrate all available information. Furthermore, differentiating between different causes of Cushing syndrome (e.g., pituitary adenoma vs. adrenal adenoma) necessitates careful interpretation of both laboratory data and imaging findings.
Diagnostic Flowchart for Suspected Cushing Syndrome
The following flowchart Artikels a typical diagnostic approach:
Suspected Cushing Syndrome?
|
V
24-hour Urine Free Cortisol
|
V
Elevated Cortisol?
Yes No
| |
V |
Low-Dose Dexamethasone Suppression Test Rule out Cushing Syndrome
|
V
Suppression?
Yes No
| |
Rule out Cushing Syndrome Further Investigations (e.g., Late-night salivary cortisol, High-resolution CT/MRI scans)
|
V
Identify Cause (e.g., Pituitary adenoma, Adrenal adenoma)
Treatment Options for Cushing Syndrome
Cushing syndrome, a condition characterized by prolonged exposure to high levels of cortisol, requires a multifaceted treatment approach tailored to the underlying cause and the severity of symptoms.
The goal of treatment is to reduce cortisol levels to a safe range, manage symptoms, and prevent long-term complications. Treatment options range from medication and surgery to radiation therapy, each with its own set of benefits, drawbacks, and potential side effects.
Medical Treatments for Cushing Syndrome
Medical management plays a crucial role in controlling Cushing syndrome, particularly when surgery is not an option or as an adjunct to surgery. Several medications are used to suppress cortisol production or block its effects. These medications work through different mechanisms and may be used alone or in combination depending on the individual’s needs and response.
Medication Types and Their Efficacy
Several medications are used to manage Cushing syndrome, each with its unique mechanism of action, efficacy, and side effect profile. For example, ketoconazole is an antifungal medication that inhibits cortisol production. Metyrapone and aminoglutethimide block cortisol synthesis at different stages. Pasireotide, a somatostatin analog, reduces ACTH secretion. These medications can effectively lower cortisol levels in many patients, but their effectiveness varies.
Some individuals may experience a significant reduction in symptoms, while others may require a combination of medications or additional treatments. The choice of medication and dosage is highly individualized and depends on various factors, including the cause of Cushing syndrome, the severity of symptoms, and the patient’s overall health. Close monitoring of cortisol levels and side effects is essential during medication therapy.
Surgical Management of Cushing Syndrome
Surgery is often the preferred treatment option for Cushing syndrome caused by a pituitary adenoma (a benign tumor of the pituitary gland) or adrenal adenoma/carcinoma (tumors of the adrenal glands). For pituitary adenomas, transsphenoidal surgery, a minimally invasive procedure, is typically performed to remove the tumor. Adrenalectomy, the surgical removal of one or both adrenal glands, is indicated for adrenal tumors.
The success of surgery depends on factors like the size and location of the tumor and the surgeon’s skill. Post-surgical monitoring is critical to ensure the effectiveness of the procedure and to detect and manage potential complications. In some cases, even after successful surgery, medication may be needed to manage residual cortisol production or to replace cortisol if both adrenal glands are removed.
Radiation Therapy for Cushing Syndrome
Radiation therapy may be used as an adjunct to surgery or as a primary treatment option in cases where surgery is not feasible or carries significant risks. Stereotactic radiosurgery, a highly precise form of radiation therapy, can be used to target and destroy pituitary adenomas. This method delivers a high dose of radiation to the tumor while minimizing damage to surrounding tissues.
The effectiveness of radiation therapy can take several months to become apparent, and it may not be effective in all cases.
Potential Complications of Cushing Syndrome Treatment
Treatment for Cushing syndrome can lead to various complications, depending on the specific approach used. Medication side effects can range from mild to severe and may include nausea, vomiting, fatigue, and liver dysfunction. Surgical complications can include bleeding, infection, and adrenal insufficiency (if adrenal glands are removed). Radiation therapy can cause headaches, nausea, and fatigue, and in rare cases, damage to surrounding tissues.
Close monitoring and prompt management of these complications are crucial to ensure the patient’s safety and well-being. Regular follow-up appointments are essential to assess treatment effectiveness and manage any potential complications.
Management of Cushing Syndrome Complications
Cushing syndrome, if left untreated, can lead to a cascade of serious health problems. Effective management involves not only controlling the underlying cause of excess cortisol but also actively addressing the complications that arise. This section details strategies for managing common complications and emphasizes the importance of lifestyle modifications and psychological support.
Hypertension Management in Cushing Syndrome
Hypertension, or high blood pressure, is a frequent complication of Cushing syndrome due to the effects of cortisol on the cardiovascular system. Management typically involves a combination of lifestyle changes and medication. Lifestyle modifications include adopting a low-sodium diet, increasing physical activity (as tolerated), and maintaining a healthy weight. Pharmacological interventions may include antihypertensive medications such as ACE inhibitors, beta-blockers, or calcium channel blockers.
Regular monitoring of blood pressure is crucial to ensure the effectiveness of the treatment plan. In some cases, surgical intervention to address the underlying cause of Cushing syndrome may be necessary to effectively control hypertension.
Diabetes Management in Cushing Syndrome
Cushing syndrome frequently leads to insulin resistance and hyperglycemia, often resulting in the development of type 2 diabetes. Management focuses on achieving and maintaining optimal blood glucose levels. This typically involves a combination of lifestyle modifications, such as a balanced diet with controlled carbohydrate intake, regular exercise, and weight management. Pharmacological interventions may include oral hypoglycemic agents or insulin therapy, depending on the severity of the condition.
Regular monitoring of blood glucose levels and HbA1c is essential to guide treatment decisions and assess treatment efficacy.
Osteoporosis Management in Cushing Syndrome
The catabolic effects of excess cortisol on bone tissue contribute to the development of osteoporosis in individuals with Cushing syndrome. Management strategies aim to prevent further bone loss and minimize fracture risk. This includes optimizing calcium and vitamin D intake through diet and supplementation. Bisphosphonates, a class of medications that slow bone loss, are often prescribed. Regular weight-bearing exercise, as tolerated, is also beneficial for bone health.
Regular bone density scans (DEXA scans) help monitor the effectiveness of treatment and identify any progression of osteoporosis.
Long-Term Health Implications of Untreated Cushing Syndrome
Untreated Cushing syndrome carries significant long-term health risks. These include an increased risk of cardiovascular disease (including heart attack and stroke), type 2 diabetes with its associated complications (such as kidney disease and nerve damage), osteoporosis with an increased risk of fractures, infections due to immune suppression, and certain types of cancers. Furthermore, the psychological impact of untreated Cushing syndrome can be severe and lead to significant impairment in quality of life.
Early diagnosis and prompt treatment are essential to mitigate these risks.
Lifestyle Modifications in Cushing Syndrome Management
Lifestyle modifications play a crucial role in managing Cushing syndrome and its complications. A balanced diet low in sodium and refined carbohydrates is essential for controlling hypertension and blood glucose levels. Regular physical activity, tailored to individual capabilities, improves cardiovascular health, aids in weight management, and strengthens bones. Stress management techniques, such as yoga or meditation, can help mitigate the psychological impact of the condition.
Weight management is crucial as obesity exacerbates many complications of Cushing syndrome. A gradual, sustainable approach to weight loss is generally recommended.
Coping with the Psychological Effects of Cushing Syndrome
Cushing syndrome can have a significant impact on mental well-being. Many individuals experience symptoms such as depression, anxiety, and mood swings. Psychological support is crucial for managing these effects. This may involve cognitive behavioral therapy (CBT), support groups, or counseling. Open communication with healthcare providers and loved ones is essential.
Learning coping mechanisms for stress management and emotional regulation can significantly improve quality of life. Understanding that these psychological effects are a common part of the condition and are treatable can be empowering for patients.
Impact on Different Body Systems
Cushing syndrome, stemming from prolonged exposure to high levels of cortisol, significantly impacts various body systems. The effects are widespread and can range from subtle changes to severe, life-threatening complications. Understanding these effects is crucial for effective diagnosis, management, and improving the quality of life for individuals affected by this condition.
Cardiovascular System Effects
Excess cortisol weakens blood vessels and increases blood pressure. This is primarily due to increased sodium and water retention, leading to fluid overload and increased cardiac workload. Furthermore, cortisol can directly stimulate the heart, increasing heart rate and contractility. These factors contribute to an increased risk of hypertension, atherosclerosis (hardening of the arteries), and cardiovascular events such as stroke and heart attack.
Individuals with Cushing syndrome may experience palpitations and shortness of breath as a result of these cardiovascular changes. Effective management of blood pressure through medication and lifestyle changes is crucial in mitigating these risks.
Musculoskeletal System Effects
Cushing syndrome significantly weakens bones, leading to a condition called osteoporotic. The excess cortisol interferes with bone formation, reducing bone density and increasing the risk of fractures. Muscle mass and strength are also diminished due to the catabolic effect of cortisol, resulting in muscle wasting (atrophy) and weakness. This can lead to mobility problems and an increased risk of falls and fractures.
Regular weight-bearing exercise and supplementation with calcium and vitamin D are often recommended to mitigate these effects. In severe cases, medications to improve bone density may be necessary.
Integumentary System Effects
The skin is profoundly affected by Cushing syndrome. The most noticeable changes include thinning of the skin, making it fragile and prone to bruising and tearing. Stretch marks (striae) often appear, particularly on the abdomen, thighs, and breasts. These are purplish-red initially, gradually fading to a lighter color. The skin may also develop a characteristic plethoric appearance, appearing flushed and red due to increased blood vessel dilation.
Acne and hirsutism (excessive hair growth) are common, particularly in women. Wound healing is often impaired due to the weakened skin and impaired immune response. Careful skin care, including moisturizing and protection from sun exposure, is essential to manage these skin changes.
Endocrine System Effects
Cushing syndrome directly disrupts the endocrine system’s delicate balance. The primary effect is the suppression of the hypothalamic-pituitary-adrenal (HPA) axis, the body’s natural feedback loop regulating cortisol production. This suppression can lead to adrenal insufficiency if the underlying cause of Cushing syndrome is not addressed. Furthermore, cortisol excess can interfere with the function of other endocrine glands, such as the thyroid and gonads, leading to secondary hormonal imbalances.
These imbalances can manifest as hypothyroidism (underactive thyroid), menstrual irregularities in women, and decreased libido and erectile dysfunction in men. Monitoring hormone levels and managing any secondary endocrine deficiencies are critical components of Cushing syndrome management.
Risk Factors and Prevention

Source: pinimg.com
Cushing syndrome, while relatively rare, is a serious condition with significant health implications. Understanding the risk factors associated with its development is crucial for implementing preventative measures and promoting early detection. This section will Artikel the major risk factors and explore potential strategies to mitigate the risk of developing this hormonal disorder.
The primary risk factor for Cushing syndrome is prolonged exposure to high levels of cortisol. This can stem from various sources, most commonly the use of glucocorticoid medications. Other factors contribute to the likelihood of developing the condition, influencing an individual’s susceptibility.
Glucocorticoid Medication Use
The most significant risk factor for Cushing syndrome is long-term use of high doses of glucocorticoid medications. These medications, often prescribed for conditions like asthma, rheumatoid arthritis, and inflammatory bowel disease, mimic the effects of cortisol. Prolonged use can lead to the body’s suppression of its natural cortisol production and ultimately, the development of Cushing syndrome. The longer the duration of treatment and the higher the dosage, the greater the risk.
For example, a patient taking high doses of prednisone for several years is at significantly higher risk than someone taking a low dose for a short period. Careful monitoring and the lowest effective dose are crucial in minimizing this risk.
Genetic Predisposition
While less common, a genetic predisposition can increase the risk of developing Cushing syndrome. Certain genetic mutations can affect the body’s ability to regulate cortisol production or its response to cortisol, making individuals more vulnerable. Family history of Cushing syndrome, although not a guarantee, should be considered a relevant factor. Further research continues to unravel the complex genetic interactions involved.
Tumors
The presence of tumors in the pituitary gland (causing Cushing disease), adrenal glands, or other parts of the body that produce or affect cortisol production is another major risk factor. These tumors can lead to excessive cortisol secretion, independent of medication use. The type and location of the tumor influence the severity and presentation of Cushing syndrome.
Lifestyle Changes to Mitigate Risk
It’s important to understand that while you cannot directly prevent genetic predisposition or the need for certain medications, adopting a healthy lifestyle can contribute to overall well-being and potentially lessen the impact of other risk factors. The following lifestyle changes may play a supportive role:
- Maintaining a healthy weight: Obesity is linked to increased cortisol levels and insulin resistance, potentially exacerbating the effects of excess cortisol.
- Regular physical activity: Exercise helps regulate stress hormones and improve overall health, potentially mitigating some risk factors.
- Stress management techniques: Chronic stress elevates cortisol levels. Practicing relaxation techniques like yoga, meditation, or deep breathing can help manage stress effectively.
- Balanced diet: A diet rich in fruits, vegetables, and whole grains, low in processed foods and sugar, supports overall health and hormone balance.
- Adequate sleep: Sufficient sleep is crucial for hormone regulation and overall well-being.
Importance of Early Detection and Intervention
Early detection and intervention are crucial for managing Cushing syndrome effectively. Early diagnosis allows for prompt treatment, minimizing the long-term complications associated with the condition. Regular check-ups, particularly for individuals on long-term glucocorticoid therapy, are essential. Recognizing the symptoms early and seeking medical attention promptly can significantly improve treatment outcomes and quality of life.
Case Studies and Examples
Understanding Cushing syndrome through real-world examples helps illustrate the diverse presentations and management challenges. This section details hypothetical and representative cases to enhance comprehension of this complex endocrine disorder.
Hypothetical Case Study: A 45-Year-Old Female with Cushing Syndrome
A 45-year-old female presents with complaints of weight gain, particularly in her face and abdomen (“moon face” and “truncal obesity”), along with purple striae on her abdomen and thighs. She reports increased fatigue, muscle weakness, and frequent bruising. Her menstrual periods have become irregular. Physical examination reveals hypertension (160/90 mmHg), hirsutism (excess facial hair), and thin, fragile skin.
Laboratory tests reveal elevated cortisol levels, both in a 24-hour urine collection and a late-night salivary cortisol test. Further investigation reveals a pituitary adenoma (a benign tumor of the pituitary gland) secreting excess ACTH (adrenocorticotropic hormone), leading to the diagnosis of Cushing disease, a form of Cushing syndrome. Treatment involves surgical removal of the pituitary adenoma. Post-surgery, her symptoms gradually improve, with normalization of cortisol levels and a significant reduction in weight and hypertension.
Varied Patient Presentations and Treatment Responses
Patients with Cushing syndrome exhibit a wide range of symptoms and severity. Some individuals may present with subtle changes, such as mild weight gain and fatigue, while others experience more dramatic symptoms, including severe hypertension, diabetes, and osteoporosis. Treatment responses are equally variable. Surgical removal of a pituitary adenoma, as in the previous case, is often successful.
However, other cases may require medication (such as ketoconazole or metyrapone to suppress cortisol production) or radiation therapy. Some patients may have a less favorable response to treatment, necessitating a combination of therapies or lifelong management of complications.
Challenges in Managing Cushing Syndrome Cases
Managing Cushing syndrome presents several challenges. Diagnosing the underlying cause can be complex, requiring multiple tests and consultations with specialists. Treatment choices depend on the underlying cause and the severity of symptoms. Monitoring treatment efficacy and managing complications (such as diabetes, hypertension, and osteoporosis) are crucial for long-term patient well-being. Furthermore, some patients may experience significant psychological impact due to the disease and its treatment, requiring psychological support.
Some tumors may be resistant to standard treatments, necessitating more aggressive interventions.
Summary of Key Features of Several Case Studies
| Case | Age/Sex | Presenting Symptoms | Underlying Cause | Treatment | Outcome |
|---|---|---|---|---|---|
| 1 | 45/Female | Weight gain, moon face, striae, hypertension, fatigue | Pituitary adenoma (Cushing disease) | Surgical removal of adenoma | Improved symptoms, normalized cortisol levels |
| 2 | 60/Male | Weight gain, diabetes, osteoporosis, easy bruising | Adrenal adenoma | Surgical removal of adenoma | Significant improvement, but requires ongoing diabetes management |
| 3 | 30/Female | Mild weight gain, fatigue, irregular menses | Ectopic ACTH secretion (lung tumor) | Chemotherapy and targeted therapy | Partial response, ongoing management required |
| 4 | 55/Male | Severe hypertension, muscle weakness, significant weight gain | Exogenous glucocorticoid use | Gradual steroid tapering | Slow improvement, careful monitoring for adrenal insufficiency |
Research and Future Directions

Source: redd.it
Cushing syndrome research is a dynamic field, constantly evolving with advancements in our understanding of its pathophysiology, diagnosis, and treatment. Current research focuses on refining diagnostic tools, developing novel therapeutic strategies, and improving long-term management of this complex condition. Significant progress has been made, yet considerable challenges remain.
Current Research Trends in Cushing Syndrome
Improved Diagnostic Techniques
Research is actively pursuing more sensitive and specific diagnostic tests for Cushing syndrome. This includes the development of improved assays for cortisol measurement, exploring novel biomarkers, and refining imaging techniques to better identify the underlying cause of hypercortisolism. For example, studies are investigating the use of salivary cortisol testing for easier and less invasive monitoring, as well as advanced imaging techniques like MRI and PET scans with higher resolution to detect smaller adrenal or pituitary tumors.
This focus on early and accurate diagnosis is crucial for timely intervention and improved patient outcomes.
Novel Therapeutic Approaches, Cushing Syndrome
The development of new therapies for Cushing syndrome is a major focus. This includes research into targeted therapies that selectively inhibit cortisol production, investigating the potential of gene therapy for correcting underlying genetic defects, and exploring innovative surgical techniques to minimize invasiveness and improve outcomes. Studies are underway evaluating the efficacy and safety of novel drugs that target specific steps in the cortisol synthesis pathway, aiming to achieve better control of hypercortisolism with fewer side effects.
Personalized Medicine Approaches
The increasing recognition of the heterogeneity of Cushing syndrome has led to a growing interest in personalized medicine. This involves tailoring treatment strategies to individual patient characteristics, such as the underlying cause of the disease, genetic background, and comorbidities. This approach aims to optimize treatment effectiveness and minimize adverse events. For example, patients with specific genetic mutations may benefit from different treatment approaches compared to those with non-genetic causes.
Areas Requiring Further Research
Several areas require further investigation to improve diagnosis and treatment outcomes for Cushing syndrome.
Long-Term Effects and Comorbidities
More research is needed to fully understand the long-term effects of Cushing syndrome and its associated comorbidities, such as cardiovascular disease, osteoporosis, and diabetes. This includes studies investigating the effectiveness of interventions to mitigate these long-term complications. Longitudinal studies following patients for extended periods are crucial to assess the impact of different treatment strategies on long-term health outcomes.
Treatment Resistance
A significant challenge is the management of patients who are resistant to conventional therapies. Further research is necessary to identify the mechanisms of treatment resistance and develop novel strategies to overcome it. This may involve investigating alternative drug targets, combining different therapies, or exploring innovative approaches like immunotherapy.
Improved Quality of Life Measures
Research is needed to develop and validate reliable and sensitive measures of quality of life in patients with Cushing syndrome. This will help to assess the impact of different treatments on patient well-being and guide the development of more effective management strategies. Standardized questionnaires and outcome measures are crucial for tracking patient progress and evaluating the overall effectiveness of interventions.
Potential Role of New Technologies and Therapies
Emerging technologies and therapies hold significant promise for improving the management of Cushing syndrome.
Minimally Invasive Surgical Techniques
Advances in minimally invasive surgical techniques, such as laparoscopic and robotic surgery, are improving the precision and safety of adrenalectomy. These techniques lead to reduced post-operative complications and faster recovery times.
Targeted Therapies and Gene Therapy
Targeted therapies, such as those inhibiting specific enzymes in the cortisol synthesis pathway, are under development. Gene therapy holds the potential to correct underlying genetic defects that contribute to Cushing syndrome, offering a more definitive cure in specific cases.
Artificial Intelligence (AI) in Diagnosis
AI algorithms may be used to analyze medical images and laboratory data to improve the accuracy and speed of diagnosis. This could facilitate earlier detection and intervention, leading to better outcomes.
Timeline of Significant Milestones in Cushing Syndrome Research
| Year | Milestone |
|---|---|
| 1932 | Harvey Cushing describes the clinical syndrome. |
| 1950s-1960s | Development of ACTH stimulation tests and other diagnostic methods. |
| 1970s-1980s | Advances in surgical techniques for adrenalectomy. |
| 1990s-2000s | Development of medications like ketoconazole and metyrapone. |
| 2010s-Present | Increased focus on personalized medicine, novel therapies, and improved diagnostic tools. |
Patient Education and Support
Source: squarespace-cdn.com
Living with Cushing syndrome presents significant challenges, impacting physical and mental well-being. Effective patient education and a strong support system are crucial for successful management and improved quality of life. Understanding the condition, treatment options, and available resources empowers patients to actively participate in their care.
Patient Education Materials
Comprehensive patient education materials should be readily accessible and tailored to different literacy levels. These materials should clearly explain the causes, symptoms, diagnostic procedures, and treatment options for Cushing syndrome. Visual aids, such as diagrams illustrating the hormonal pathways involved, can enhance understanding. Information should also cover potential complications, self-management strategies, and the importance of regular follow-up appointments.
Materials should be available in multiple formats, including print, online, and video, to cater to diverse learning preferences. The inclusion of patient testimonials can offer comfort and reassurance.
The Role of Support Groups and Patient Advocacy Organizations
Support groups and patient advocacy organizations provide invaluable emotional, informational, and practical support for individuals with Cushing syndrome and their families. These groups offer a safe space to share experiences, exchange coping strategies, and connect with others facing similar challenges. They can also provide access to resources, such as financial assistance programs, and advocate for improved patient care and research funding.
Examples of these organizations include national and international patient advocacy groups dedicated to endocrine disorders, which often have specific support networks for Cushing syndrome patients. These groups often host online forums, in-person meetings, and educational events.
Ongoing Monitoring and Follow-Up Care
Regular monitoring and follow-up care are essential for managing Cushing syndrome and its complications. This includes regular appointments with an endocrinologist to assess hormone levels, monitor for side effects of treatment, and adjust medication as needed. Patients should be educated on the importance of reporting any new or worsening symptoms promptly. Regular monitoring may involve blood tests, urine tests, imaging studies, and physical examinations to assess overall health and detect any potential complications early.
The frequency of follow-up appointments will vary depending on the individual’s condition and response to treatment.
Resources Available to Patients and Their Families
Numerous resources are available to support patients and their families navigating the challenges of Cushing syndrome. These include:
- Endocrinology clinics and specialists: These provide expert medical care and management of the condition.
- Patient advocacy organizations: These offer emotional support, information, and resources.
- Online support groups and forums: These provide a platform for sharing experiences and connecting with others.
- Governmental and non-profit organizations: These may offer financial assistance programs or other support services.
- Educational materials: These are available from various sources, including medical institutions and patient advocacy groups.
Access to these resources can significantly improve the quality of life for individuals with Cushing syndrome and their families, facilitating effective management of the condition and its impact.
Closure
Successfully navigating Cushing Syndrome requires a multi-faceted approach encompassing accurate diagnosis, tailored treatment strategies, and proactive management of complications. Early detection and intervention are paramount in minimizing long-term health consequences. By understanding the diverse manifestations of this condition, employing effective diagnostic tools, and utilizing appropriate treatment options, we can significantly improve the quality of life for individuals living with Cushing Syndrome.
Remember that ongoing monitoring and patient education are key components of successful long-term management.
